Listening to Our Gut: How Genomic Sequencing of the Gut Microbiome Is Advancing Human Health
The status of gut microbiome research and where innovation is needed
Interest in how the gut microbiome impacts human health is rising. There has been a surge in consumer products from yogurts to gut shots that claim to “improve” the microbiome, as well as a huge uptake of home testing kits that promise personalized nutrition advice based on your gut microbiome.
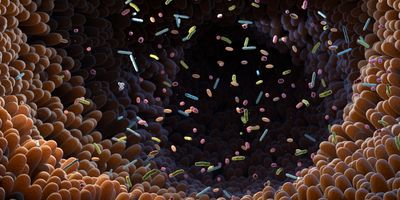
However, the reality is somewhat more complex. The tiny tenants in our gut are made up of hundreds to thousands of species of bacteria, archaea, fungi and viruses, weighing around 500g. Initial research shows that gaining the right microbial balance has the potential to boost immunity, overcome food intolerances, and even increase energy levels. But realizing these benefits requires a much deeper understanding of the gut's diverse species and their roles.
Researchers’ grasp of the link between gut microbes and overall health is still premature. Early breakthroughs in unravelling microbial biology have been powered by genomics. But there’s still a lot to be learned. A 2020 study that sequenced genomes from 200,000 gut microbiomes found that 70 percent of the microbial populations it analyzed had never been cultured before.
So, how advanced is research in the field currently? How are microbiome samples actually sequenced, and what developments are needed to scale and accelerate innovation in the field?
The science behind your samples
Testing the gut microbiome typically involves taking a feces sample that is genetically sequenced using one of two main approaches. The first is amplicon-based sequencing a cost-effective way to identify which species of microbes are present. Researchers begin by selecting a target region of DNA or RNA. Often, these regions are specific to a group of organisms, such as the 16S rRNA gene in bacteria. This uniqueness means the target region acts like a barcode for researchers to identify the variety of microbes in a sample. Since prior knowledge of microbes is required to identify them, amplicon-based sequencing isn’t the best option for characterizing newly discovered species. The downside to this approach is that it doesn’t reveal much about the microbes’ functions.
The second approach is shotgun metagenomics. While amplicon-based sequencing targets a specific region of DNA, shotgun sequencing captures all the DNA present in the sample, attempting to represent the entire microbial community. Extracted DNA is randomly cut into many fragments and sequenced. Sequences are then either computationally assembled or sequences are mapped without assembly, and bioinformatics tools reveal areas of overlap and match them against reference genomes to confirm the microorganisms present in the sample.
Shotgun metagenomics sequencing provides a deeper analysis of samples, identifying subspecies or strains, rather than just genus or species. Gene expression and function can also be analyzed to give insight into how metabolic functions contribute to community fitness, host-microbe interactions, and symbiosis. For example, shotgun sequencing can reveal the presence of genes involved in antibiotic resistance or metabolism. However, shotgun sequencing carries greater bioinformatics cost and resourcing needs, as it sequences all the DNA in a sample rather than just target regions.
The method researchers choose depends on the goals and size of their project. Amplicon-based sequencing is useful for comparing the composition of microbial communities in different environments. When it comes to deepening knowledge of the role microbes play in human health, shotgun metagenomics’ detailed analysis is critical.
From data to drugs: microbiome applications
A growing understanding of the variety and function of gut microbes has begun to enable several human health applications. A notable example from 2023 is the FDA’s approval of the first oral drug designed to alter the microbiome to prevent recurring C. difficile infections (CDI). A potentially life-threatening condition, CDI spreads easily in hospitals and often infects people who have recently taken antibiotics. Since antibiotics kill other bacteria in the gut, CDI can quickly grow out of control. C. difficile spores are resistant to heat, acid, and many antibiotics and disinfectants, making treating the infection extremely challenging.
The new drug works by restoring the population of beneficial bacteria in the gut to prevent C. difficile from thriving and infection recurring. A significant majority (88 percent) of patients who received the drug did not have an infection eight weeks after a single course of treatment – the critical period for recurring infections. The approval of SER-109 opens the door to a new way of thinking about microbiome-related conditions—fighting microbes with microbes.
The road ahead for microbiome research
As researchers learn more about the biology of the gut microbiome and its link to human health, new possibilities for advancing and personalizing treatments are being unlocked. But it’s going to take more than just a yogurt or a “miracle” gut shot to truly realize the hype around the microbiome.
Advances in sequencing technology will continue to be the driving force behind microbiome research breakthroughs. Previous hurdles are being overcome with increased accuracy, easier workflows, and more advanced bioinformatics. For example, in shotgun metagenomics, HiFi technology makes it possible to recover DNA in larger fragments, or even sometimes assemble an entire microbial chromosome in one contig. Having fewer fragments and better bioinformatics tools is simplifying the process of piecing DNA back together. This results in fewer errors and a deeper analysis of microbes in the sample. The cost of sequencing is also decreasing exponentially, with smaller samples needed to generate results.
By investing in the latest sequencing technology, researchers can make leaps in gut-related health conditions that were once challenging to tackle and unlock the promise of precision treatments.